Uncategorized
What are the causes smoking cannabis
Health outcomes associated with long-term regular cannabis and tobacco smoking. Cannabis smoke contains a similar profile of carcinogenic chemicals as tobacco smoke but is inhaled more deeply.
Abstract
The respiratory health effects from tobacco smoking are well described. Cannabis smoke contains a similar profile of carcinogenic chemicals as tobacco smoke but is inhaled more deeply. Although cannabis smoke is known to contain similar harmful and carcinogenic substances to tobacco smoke, relatively little is understood regarding the respiratory health effects from cannabis smoking.
There is a need to integrate research on cannabis and respiratory health effects so that gaps in the literature can be identified and the more consistent findings can be consolidated with the purpose of educating smokers and health service providers.
This review focuses on several aspects of respiratory health and cannabis use (as well as concurrent cannabis and tobacco use) and provides an update to (i) the pathophysiology; (ii) general respiratory health including symptoms of chronic bronchitis; and (iii) lung cancer.
Cannabis Use and Respiratory Impairment—Why the Concern?
Cannabis is the most commonly used illicit substance across the globe, particularly among adolescents. The drug is derived mainly by drying and pressing the Cannabis sativa plant which can be grown in various climates; it is often grown indoors. The drug is most commonly smoked in a hand-rolled cigarette (referred to as a joint) or in a designed water pipe (referred to as a bong); it may also be added to food and eaten.
Cannabis contains many chemicals unique to the plant (referred to as cannabinoids), including the desired psychoactive component—delta-9-tetrahydrocannabinol (THC). Approximately one in 10 Australians over the age of 14 years has used cannabis at least once in the previous 12 months (12.9% of males and 7.7% of females). Notably, approximately one in 10 individuals who ever smoke cannabis will experience a dependence syndrome.
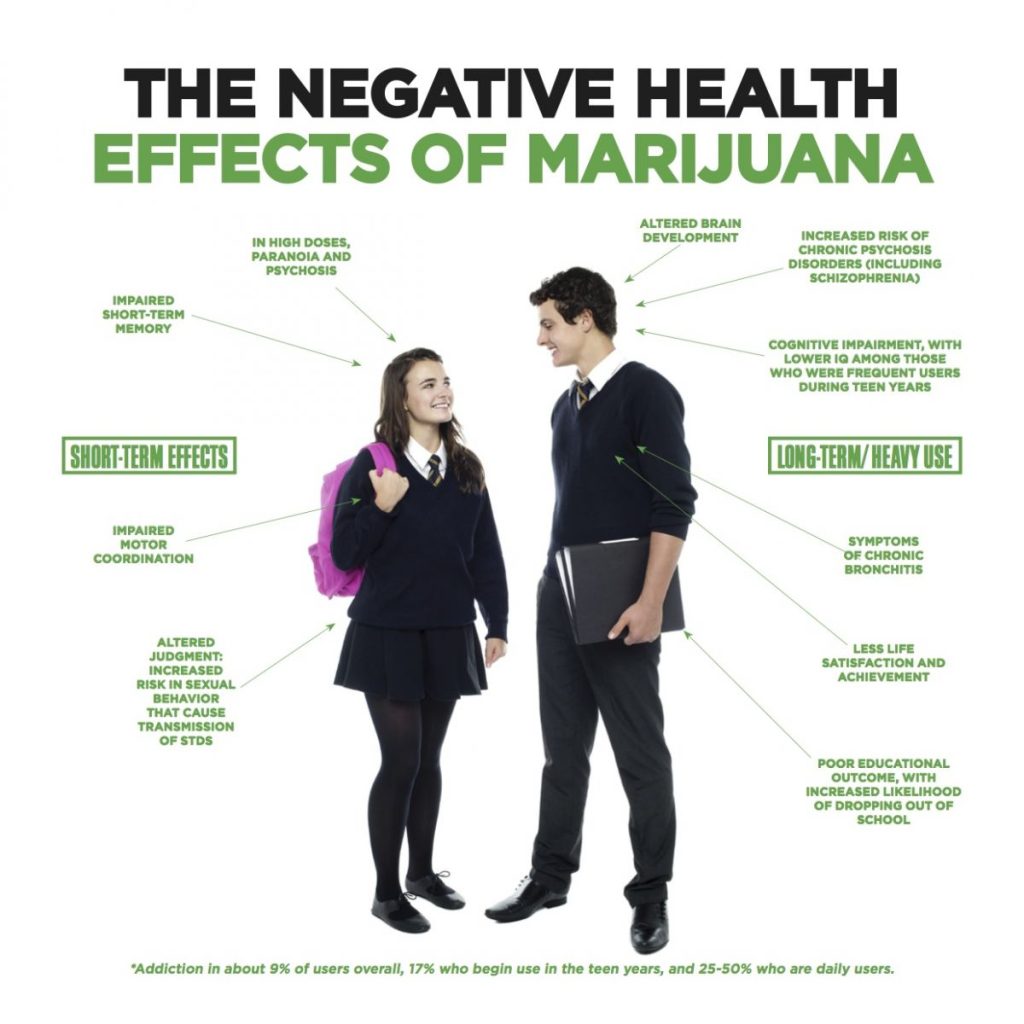
The most commonly occurring harms associated with regular use include an increased risk of developing psychotic symptoms and disorders, impaired educational attainment, use of other illicit drugs and respiratory impairment. These are significant harms with cannabis dependence accounting for 10.3% of illicit drug dependence burden worldwide and an estimated loss of 7000 disability-adjusted life years due to the risk of impacting on the prognosis of schizophrenia.
Cannabis smoke is known to contain a similar array of harmful and carcinogenic chemicals to that of tobacco smoke. Concerns regarding the respiratory effects of inhaling cannabis smoke, as a product of combustion in a pipe, joint or bong, are heightened by the knowledge regarding the harm caused by tobacco smoke and the different way in which cannabis is smoked.
That is, when smoking cannabis compared with tobacco, there is a prolonged and deeper inhalation and it is smoked to a shorter butt length and at a higher combustion temperature. This inhalation technique results in an approximately fivefold increase in carboxyhaemoglobin concentration, fourfold greater amount of tar inhaled and the retention of one third more tar in the lower airway.
To date, a number of informative literature reviews have considered the respiratory health effects of cannabis smoke, including a position paper by the Thoracic Society of Australia and New Zealand (2003) and a recent account by Tashkin. This review provides a current understanding of the research concerning the associations between cannabis use and respiratory impairment.
Some initial considerations
Before considering the literature on the effect of cannabis smoking on respiratory health, it is important to understand some limitations to the research discussed in this article. First, the great majority of studies focus on the frequency of substance use (typically reporting the number of smoking days), and largely ignore the impact of the quantity of cannabis leaf in each joint (joint size), the proportion of each joint which is smoked (puff duration/volume/intensity) and the possibility of sharing joints.
This limitation may be particularly important to respiratory health research as study of tobacco smoking has shown that the quantity of tobacco that is inhaled is an independent predictor of negative respiratory outcomes in addition to the frequency of inhalation. Some initial cannabis-related web-based research supports this finding.
That is, an online survey of 5987 adults in the US who reported at least monthly cannabis use was conducted that included a measure of quantity of cannabis (quarter ounces per month and levels of intoxication) and frequency of cannabis use. Importantly, both the quantity and frequency of cannabis used were independently and significantly associated with an increased number of respiratory problems.
In addition to quantity, the impact of duration of smoking (cannabis use history) is also often ignored in place of frequency of past year use. Notably, quantity and frequency of cannabis use as well as duration of use are important and independent predictors of cannabis dependence, and general health concerns.
Finally, when comparing tobacco and cannabis smoking, it is important to note that, in addition to the differences in inhalation techniques already described, tobacco cigarettes are typically smoked in greater frequency, albeit with shorter puff duration (possibly due to the half-life of nicotine; approximately 2 h23 compared with almost 1 week for cannabinoids), compared with cannabis joints and thus have an imbalanced effect when these substances are compared solely by days of use.
For these reasons, considering only frequency as a variable in the absence of quantity or duration of use in research studies may lead to false negative associations between smoking and health outcomes.
Second, as cannabis is most commonly smoked by the joint (cigarette), there is a corresponding lack of research on the impact of using differing routes of administration such as water pipe or vaporizer. Some initial research which has recognized this limitation includes a comparison of the toxic outputs of vaporizers and water pipes conducted by the National Organization for the Reform of Marijuana Laws.
In this study on the toxin levels produced by combusted and vaporized cannabis, the vaporizer but not water pipe was shown to reduce toxins compared with joint smoking. This finding was in line with separate recent study which identified that vaporizer users perceive them to have respiratory harm-reducing effects.
Notably, although the respiratory effects of vaporizing cannabis are likely to be reduced, other study has shown that vaporizing cannabis can produce significant levels of the neurotoxin ammonia.
Third, there is a general uncertainty of the significance of cannabis potency, or THC content, on health outcomes. Moreover, the average user typically cannot reliably identify the particular dose of the cannabis which they smoke.
Unfortunately, research on the impact of cannabis potency on public health is rare and is currently limited to demonstrated links with cannabis dependence, increases to treatment seeking for cannabis-related problems, and vulnerability to psychosis.
Finally, there is a lack of research which isolates the impact of cannabinoids other than the most commonly considered and psychoactive component of cannabis, THC, such as cannabidiol (CBD), although interest in CBD as an anti-inflammatory and anti-oxidant is starting to grow.
In regards to respiratory health, this is of particular concern as early evidence using animal models suggests that CBD can inhibit bronchoconstriction which may be an important protective mechanisms against aero-allergens. The inhibitory effects of CBD on bronchoconstriction were shown to be complex and dependent on dose.
That is, the described impact was most significant at 1 mg/kg, while, paradoxically, a higher dose of 10 mg/kg caused bronchoconstriction. As such, the individual cannabinoids in the cannabis plant may act on respiratory health in a complex and integrative manner meaning that one should not consider that any two plants will have an exactly equivalent effect on respiratory health.
Acute Effects of Cannabis Use on Respiratory Health
The acute effects of cannabis use on respiratory health are considered to impact most strongly on bronchial dynamics. Upon smoking cannabis, there is evidence of an immediate decrease to airway resistance due to bronchodilation, which may be dose related.
The mechanism causing bronchodilation is not well understood; however, animal studies have shown that anandamide (an endogenous cannabinoid) is synthesized in lung tissue and activates cannabinoid receptors (namely CB1) which, when bronchial muscle is contracted, can inhibit this constriction.
This response is likely to peak at 15 min and last for approximately 1 h46 and may partially explain the early use of cannabis as a treatment for asthma in the nineteenth century. Notably, in the case where the bronchial muscle is relaxed, anandamide was seen to cause bronchospasm.
An action that the authors state may contribute to the negative effects on the respiratory system following long-term frequent cannabis use (referred to as chronic use), which are reviewed here.
Chronic Cannabis Use and Airway Inflammation and Infection
Cannabis smoking is likely to result in airway inflammation and infection. First, cannabinoids are known to be an immune modulator through endocannabinoid receptors present in many pathways of the immune system.
Second, cannabinoids have been shown to affect the functioning of immune cells such as B and T lymphocytes, and natural killer cells.
Third, they can alter the expression of many cytokines such as interleukin (IL)-6, IL-8, IL-10, IL-12, tumour necrosis factor-alpha and interferon-gamma.
Fourth, alveolar macrophages are found in greater quantity among tobacco and cannabis smokers compared with non-smokers. Moreover, studies have suggested that cannabinoids affect macrophage functioning such as suppressing phagocytosis, spreading and bactericidal activity.
Nitric oxide production by macrophages, essential for effective bacterial killing, has also been shown to be affected by cannabinoids.
Finally, cannabis smoking is also associated with tracheobronchial mucosal injury potentially increasing the susceptibility of the airway to bacterial or viral infection. There is some evidence that this injury may follow oxidative stress caused by pyrolysis products produced in the presence of cannabinoids in the cannabis smoke.
A large body of observational work also supports the link between cannabis smoking and airway inflammation and infection.
First, there is consistent evidence that cannabis smoke is associated with inflammation of the airways with an increased visual bronchitis score (diagnosed by bronchoscopic inspection) to a similar magnitude to that which is associated with tobacco smoke.
Second, airway biopsies of marijuana smokers have demonstrated evidence of vascular hyperplasia, submucosal oedema, inflammatory cell infiltrates, basement membrane thickening and goblet cell hyperplasia.
Furthermore, bronchoalveolar lavage demonstrated increased neutrophils and IL-8 levels, particularly in those who combined marijuana and tobacco.
Third, there is some evidence of an increased risk of respiratory infection among cannabis smokers compared with non-smokers, particularly among cross-sectional samples of individuals seropositive for human immunodeficiency virus.
In contrast, this increase of risk was not seen in a 1.5-year longitudinal multicentre study of homosexual men that assessed substance use in the past 2 years.
Finally, data from outpatient medical centres have shown that cannabis-only smokers compared with non-smokers were more likely to enter these services for respiratory illnesses over a 2-year period.
A recently emerged cause for concern is the effect of various forms of contamination present on the cannabis plant before it is dried and pressed. Indeed, due to evidence of high toxicity, respiratory protection is advised to police officers in order to prevent exposure during investigations of indoor grow operations.
Further, there has been call for routine testing of cannabis grown for medicinal purposes in the US due to findings of several contaminants not visible to the naked eye. In particular, Aspergillus fumigatus is prevalent on cannabis grown in indoor environments.
To date, there have been several case reports of lung infection following the smoking of cannabis contaminated with this fungus and, more recently, with talcum dust. Aspergillus fumigatus can cause allergic bronchopulmonary aspergillosis in patients with asthma and cystic fibrosis.
Unfortunately, the prevalence and significance of the effects of smoking contaminated cannabis is yet to be the focus of any larger study.
Chronic cannabis use and general respiratory health
Population-based studies that control for tobacco smoking have consistently reported a higher frequency of cough and sputum production and wheezing among regular cannabis smokers compared with non-smokers.
Some of these studies have identified that these symptoms occur only to a similar extent as seen in tobacco-only smokers and were not additive, and one study found these symptoms were greater among tobacco-only smokers compared with cannabis-only smokers.
In addition, one novel longitudinal study of 299 individuals spanning an average of 8–12 years showed that these symptoms were reduced to non-smoker levels upon cessation of use.
A growing body of literature has assessed the impact on lung function of cannabis use in terms of chronic obstructive pulmonary disease (COPD), most commonly by measuring the forced expiratory volume in 1 s (FEV1) and forced vital capacity (FVC).
Using these measures, a few studies have found a relationship between regular cannabis use and increased airway obstruction compared with those who do not use (this relationship was found only for men in an additional two studies, although one did not find a reduction in FEV1, but reported a reduced FEV1 : FVC ratio evidencing a possible precursor of airway obstruction).
In contrast, several studies have found no such relationship, while others report decreased obstruction (although one such study was of a synthetic THC aerosol rather than cannabis smoking).

I was really surprised at how well they work. I amp my microdosing with them and it is fantastic. Haven’t taken a real ride yet but judging from the small amounts I am taking, and are working great, the larger doses will undoubtedly be a nice lift off
This is very educational